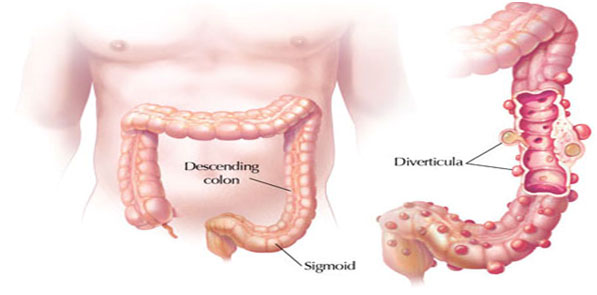
Stoma is a surgically created opening between an internal organ and the body surface. Stoma may often be created as a part of intestinal surgery when there must be a new way for waste
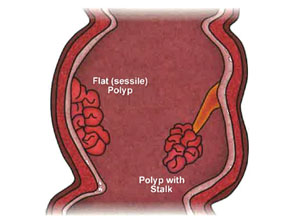
products to leave the body. Cancer, trauma, inflammatory bowel disease (1BD), bowel obstruction, infection, faecalincontinence (inability to control bowel movements) and diverticulitis
(inflammation of tiny pockets that commonly form in the colon wall) are all possible reasons for Stoma creation.
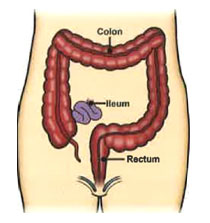
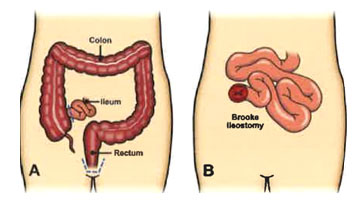
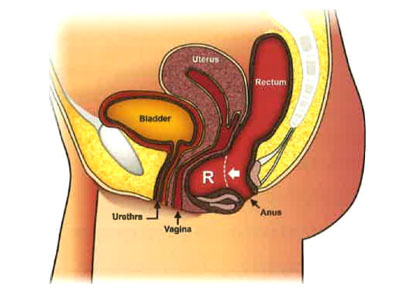
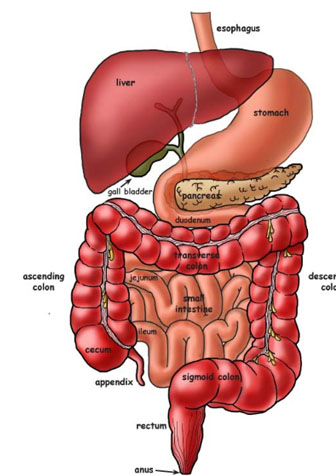
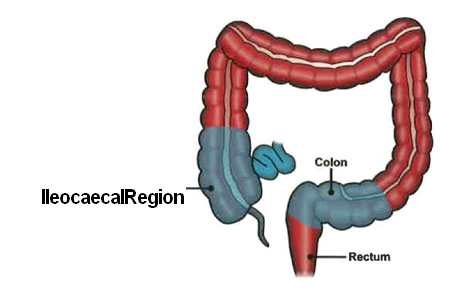
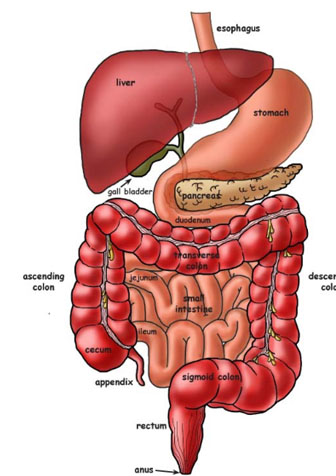
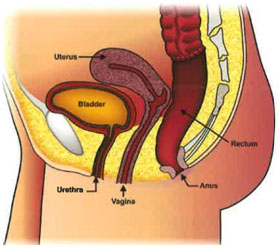
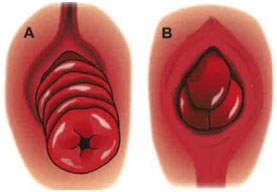
The most common types of stomas include: "ileostomy" (which connects the ileum, the last part of the small intestine, to the skin of the abdominal wall) and "colostomy" (which connects a
part of the colon, or large intestine, to the skin of the abdominal wall).
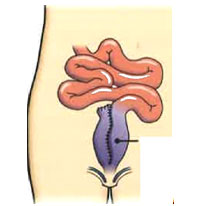
A Stoma may be temporary or permanent. A temporary stoma can usually be reversed. It is created to temporarily keep stool material away from a downstream area (closer to the anus), such as
a healing surgery site, an area of inflammation, or a blockage associated with disease or scar. A permanent stoma may be needed when disease, or its treatment, impairs normal intestinal
function, or when the muscles that control elimination must be removed or no longer work properly.
How will I control my bowel movements?
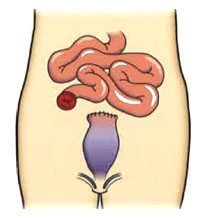
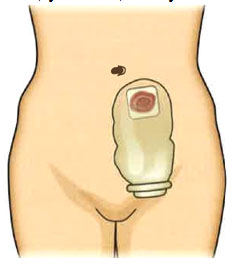
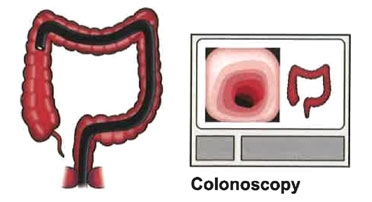
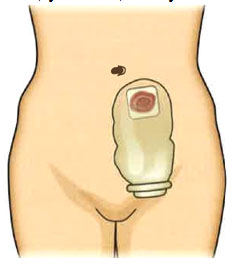
Once a stoma is created, your bowel movements will naturally empty through the stoma. A pouch, called a stoma appliance, is typically worn on the outside of your body around the opening.
The appliance isdesigned to catch and hold the emptied stool. A stoma therapist nurse who specializes in stoma care and your colorectal surgeon will teach you how to attach the appliance.
The pouch (bag) is made of plastic and is held to the body with an adhesive, which, in turn, protects the skin from moisture. The pouch is disposable and is emptied or changed as needed.
The system is quite secure; "accidents" are not common, and the pouches are odour-free.The frequency and quantity of your bowel movements will vary, depending on the type of ostomy you
have, your diet, and your bowel habits prior to surgery.
A stoma connects either the small or the large intestine to the surface of the body.
Will my diet be limited?
You may be instructed to modify your eating habits in order to control the frequency and consistency of your bowel movements, depending on the type of your stoma. Chew your food well and
drink plenty of fluids. You may be asked to avoid certain high roughage foods. Over time, most patients can introduce foods back into your diet a little at a time and monitor the effect of
each food on the stoma function. Most patients will eventually have no limitations. Your stoma nurse and colorectal surgeon will give you more details.
Will other people know that I have a stoma?
Not unless you tell them. An stoma is easily hidden by your usual clothing. You probably have met people with a stoma and not realized it!
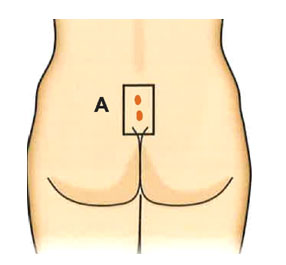
Where will the stoma be located?
A stoma is best placed on a flat portion of the abdominal wall that can be easily seen and reached by you. Before surgery, it is best for your stoma nurse to mark an appropriate place on
your abdominal wall. A colostomy is usually placed to the left of your belly button and an ileostomy to the right.
Will my physical activities be limited?
All your activities, including active sports, may be resumed once healing from surgery is complete. Public figures, footballers, prominent entertainers, and even professional athletes have
stoma that do not significantly limit their activities.
Will a stoma affect my sex life?
Most patients with stoma resume their usual sexual activity. Some patients worry about how their sexual partner will think of them because of their stoma appliance. This perceived change
in body image can be overcome by a strong relationship, time and patience.
What are the complications of an stoma?
Complications from a stoma can occur. When you first start working with your stoma, it may take some time for you tolearn how the stoma works and how the appliance fits and empties. During
this time, there may be occasions when "accidents" happen. Once you have adjusted to the appliance, the most common complications related to the stoma are minor, like local skin
irritation, and can be easily remedied.
Significant changes in body shape, such asweight loss or gain, can affect the function of a stoma. Other problems that occur over time may include hernia (weakening of the abdominal wall
around the stoma) or prolapse (a protrusion of the bowel), that occasionally require surgery if they cause significant symptoms.
Living with a stoma will require some adjustments and learning, but an active and fulfilling life is expected. Your stoma nurse and colorectal surgeon will provide you with skills and
support to help you live withyour stoma.